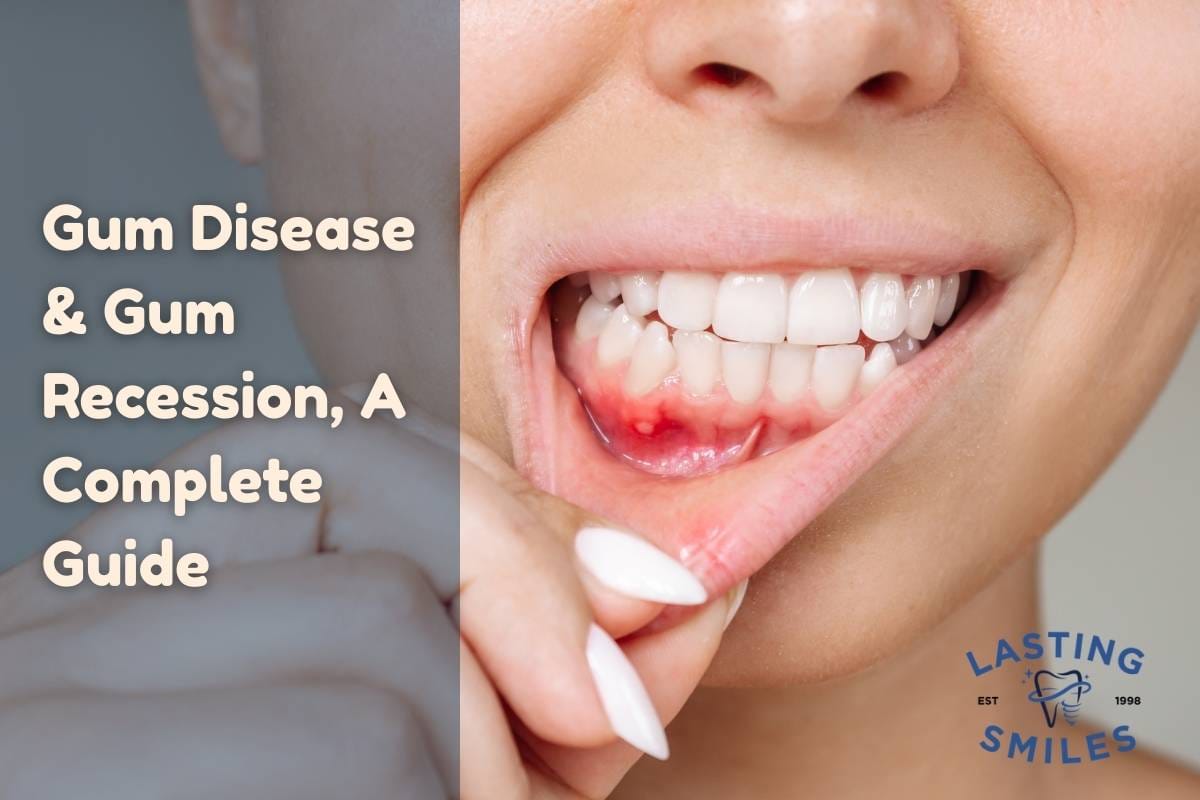
Gum disease (also called periodontal disease) is a major oral health concern that affects millions worldwide. It involves inflammation and infection of the tissues that support the teeth. When left unchecked, it can lead to gum recession, bone loss, tooth mobility, and even tooth loss.
In this article, you’ll learn:
- What gum disease and gum recession are
- Early signs and symptoms to watch for
- Underlying causes and risk factors
- Diagnosis and assessment methods
- Treatment approaches (nonsurgical & surgical)
- Prognosis and maintenance
- How gum disease relates to dental implants
- How Lasting Smiles supports patients with periodontal concerns
Throughout the post, I’ll use synonyms and varied phrasing to maintain readability and SEO value. I’ll also insert internal hyperlinks to relevant service pages on your site to deepen engagement and SEO strength.
What Is Gum Disease & Why Does Recession Happen?
Periodontal disease is an infection of the gums and supporting structures around the teeth, caused by bacterial plaque. In its early phase, it’s called gingivitis, characterized by gum swelling and bleeding. As it progresses, it becomes periodontitis, leading to attachment loss, formation of deep pockets, bone deterioration, and possibly gum recession.
Gum recession, or gingival recession, refers to the retreat of the gum margin from the tooth, exposing root surfaces. Root exposure increases sensitivity, risk of root decay, and aesthetic concerns. Once recession occurs, the lost tissue generally cannot regenerate on its own without intervention.
Because healthy gums are essential for stable dental work, controlling and treating gum disease is critical—especially before considering dental implants.
Early Warning Signs & Symptoms to Watch For
Detecting gum disease early improves outcomes significantly. Watch for:
- Gums that bleed when brushing or flossing
- Red, tender or swollen gums
- Persistent bad breath or unpleasant taste
- Gum margin that looks withdrawn, with roots becoming visible
- Teeth that appear longer than before
- Tooth sensitivity to hot, cold, sweet foods
- Deepening gum pockets when probed
- Loose or shifting teeth
- Pus or discharge around gum crevices
If you notice any of these signs, don’t delay — early assessment by a dentist or periodontist is vital.
Underlying Causes & Risk Factors
Gum disease and recession are multifactorial. Some major contributors include:
- Accumulation of plaque and tartar — bacterial biofilm irritates gum tissue
- Aggressive brushing or abrasive brushing techniques
- Misaligned bite or malocclusion, causing uneven pressures
- Teeth grinding or clenching (bruxism)
- Genetic predisposition — some people have thinner tissue or weaker defenses
- Smoking / tobacco use — reduces healing and increases disease risk
- Hormonal changes, immune conditions, chronic illness (e.g., diabetes)
- Poor dental restorations (roofs, crowns, bridges) with rough edges or margins under the gum
- Inadequate oral hygiene habits
- Periodontal pockets / deep gum infection breaking down support
Because many patients have multiple overlapping risk factors, a holistic approach is necessary when planning treatment.
Diagnostic & Assessment Tools
To evaluate gum tissue health and plan treatment, clinicians use:
- Probing with a periodontal probe — measuring pocket depths around each tooth (healthy 1–3 mm; diseased >4 mm)
- Recession measurement — distance from cementoenamel junction (CEJ) to gum margin
- Gum thickness and biotype assessment
- Gingival attachment and mobility testing
- Radiographs (X-rays) to visualize bone levels and detect bone loss
- Digital imaging / CBCT in advanced cases, especially when planning grafting or implants
This thorough diagnostic work is frequently performed before implant treatment to ensure a stable foundation.
Treatment Strategies: Conservative to Surgical
Depending on severity, the treatment spectrum ranges from noninvasive to surgical. Most effective programs combine multiple methods.
Nonsurgical / Conservative Options
These treatments aim to control infection, reduce bacterial load, and halt progression:
- Scaling & Root Planing (Deep Cleaning)
Removal of plaque and tartar beneath the gumline, smoothing root surface to encourage reattachment. - Antimicrobial / Antibiotic Therapy
Local or systemic medications to suppress bacterial populations. - Desensitizing Agents / Fluoride Applications
To reduce sensitivity in areas of exposed root surfaces. - Composite Root Covering / Bonding
Applying tooth-colored resin over exposed areas to protect roots and improve aesthetics. - Occlusal Adjustment / Splinting
Managing bite discrepancies or distributing forces evenly.
These approaches are often sufficient in early to moderate disease stages and may reduce or delay the need for surgery.
Surgical & Regenerative Techniques
When conservative measures are inadequate, more advanced interventions can restore tissues or prevent further loss:
- Gingival (Gum) Grafting
Soft tissue grafts (connective tissue graft, free gingival graft) from your palate or donor sources to cover roots and thicken gum margins. - Pinhole Surgical Technique / Minimally Invasive Graft Methods
Less invasive options to reposition gum tissue without large incisions. - Guided Tissue Regeneration (GTR)
Using membranes and graft materials to encourage rebuilding of bone and soft tissues. - Bone Grafting / Ridge Augmentation
Especially when gum loss is accompanied by bone deficiencies. This is frequently done before or in conjunction with implant planning — see our quality implant treatments. - Flap surgery / pocket reduction procedures
Exposing hidden areas for cleaning and repositioning gum margins.
Post-surgery, healing protocols include careful cleaning regimens, avoiding trauma, and follow-up visits to monitor success and stability.
Prognosis, Maintenance & Longevity
The long-term success of periodontal therapy depends heavily on:
- Thorough removal of bacterial irritants
- Strict oral hygiene habits
- Regular professional maintenance visits
- Control of risk factors (e.g., quitting smoking, managing systemic disease)
- Frequent monitoring and early intervention for relapse
For many patients, gums can stabilize, pockets reduce, and further recession may be prevented indefinitely.
If you also plan on getting implants later, managing gum disease first is crucial to implant longevity and health.
Gum Disease, Recession & Dental Implants: The Connection
A healthy gum and bone foundation is essential for successful implant therapy. Uncontrolled periodontal disease increases the risk of peri-implantitis (infection around implants). Some key points:
- Implants placed into infected or inflamed sites are at higher risk of failure.
- Patients with a history of periodontitis require more intensive maintenance after implant placement.
- Soft tissue grafts and bone augmentation are often used to strengthen the site before placing implants.
- For full-arch solutions—like All-on-X systems or 3-on-6 implants—managing and stabilizing gum health is a pre-requisite.
For more about how grafting integrates with implants, see our pages on grafting & quality implant treatments.
Prevention Is the Best Strategy
Because gum disease is preventable, aggressive care and habit management are your strongest defenses:
- Brush twice daily with a soft-bristled toothbrush
- Floss or use interdental cleaners daily
- Use antimicrobial or antiseptic mouth rinses
- Attend regular professional cleanings (every 3–6 months or per risk level)
- Avoid tobacco use
- Wear a nightguard if you grind or clench your teeth
- Ask your dentist to check the fit and margins of crowns, bridges, and orthodontic appliances
- Monitor for early signs (bleeding, swelling, sensitivity) and act swiftly
Well-maintained gums support healthy teeth, implants, and overall oral comfort.
FAQ — Common Questions About Gum Disease & Recession
Can gums grow back on their own?
No. Once gum tissue recedes, it does not regenerate naturally. Surgical or grafting intervention is required to restore the lost tissue.
Is gum disease curable?
Periodontal disease can be controlled and remission achieved, but it cannot be “cured” like a one-time fix. Long-term maintenance is essential.
How fast does gum disease progress?
It varies by individual. Some progress slowly over years; others with risk factors may advance more rapidly. That’s why early intervention is key.
Does recession always mean bone loss?
Often yes—gum recession may indicate loss of underlying bone. Radiographs help confirm bone levels.
Are grafts painful?
Modern gum grafting methods are relatively comfortable. Discomfort is manageable with sedation, pain medication, and proper post-op care.
Can I prevent gum disease?
While you may have genetic risk, you can greatly reduce chances by brushing gently with soft bristles, flossing daily, attending regular cleanings, and avoiding tobacco.
If I already had implants or full-arch work, can I still have gum disease?
Yes. Even mouth restorations like All-on-X or 3-on-6 implants depend on healthy surrounding gum tissues. That’s why we always evaluate and treat gum health as part of implant planning.
Summary & Takeaway
- Gum disease is an infection and inflammation affecting gums and supporting bone.
- Gum recession is the downstream effect of untreated disease or traumatic factors.
- Early symptoms include bleeding, sensitivity, and pocketing.
- Treatment ranges from noninvasive deep cleanings to surgical grafts and regeneration.
- Control and maintenance are crucial for long-term success.
- Healthy gums are essential before placing implants or advanced restorative work.
- Lasting Smiles integrates periodontal therapy with implant care to deliver stable, long-term results.
If you suspect gum disease or are planning dental implant work, reach out to us for a comprehensive consultation and evaluation. Let us help you restore and maintain healthy gums, confident smiles, and lasting oral health.
Recent Articles
Different Types of Dentures in Irvine: Your Complete Guide to Choosing the Best Option for Your Smile
For thousands of patients, dentures remain one of the most reliable, life-changing solutions for restoring confidence, chewing ability, and overall oral function. At...
Removable Veneers vs. Permanent Veneers: Which Option Is Right for Your Smile?
In recent years, removable veneers—often promoted on social media as a quick, inexpensive way to achieve a “perfect smile”—have gained massive attention. TikTok...
Sedation Dentistry in Irvine, CA: Relaxed, Comfortable Dental Care at Lasting Smiles
For many people, visiting the dentist can trigger anxiety, fear, or even panic. Whether it stems from a past traumatic experience, fear of...