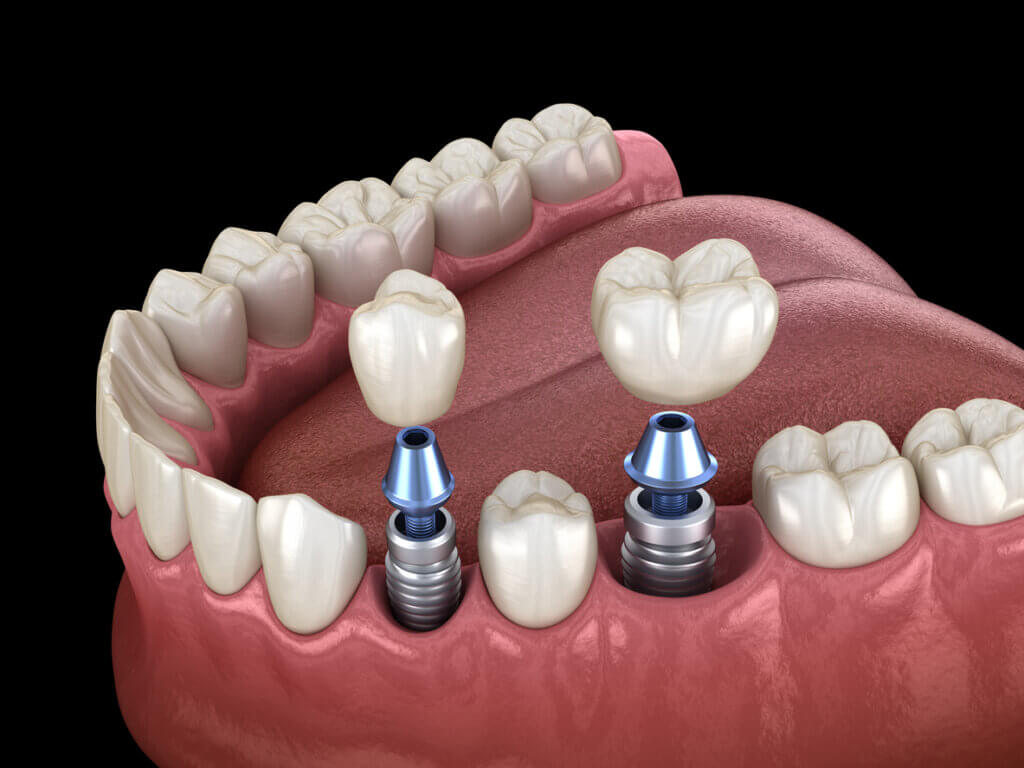
Dental implants are a great solution for replacing missing teeth and restoring your smile. They are durable, natural-looking, and comfortable. Dr. Ghodsi, a distinguished dental implant specialist at Lasting Smiles Dental Care in Las Vegas and Pasadena, has over 30 years of experience and more than 10,000 successful implant cases. He provides his patients with durable, natural-looking, and comfortable dental implants. However, like any dental procedure, they require proper care and maintenance to avoid complications. One of the most serious problems that can affect dental implants is peri-implantitis (PI).
What is Peri-Implantitis?
Peri-implantitis is a destructive inflammatory process that affects the soft and hard tissues surrounding dental implants. It is caused by bacterial plaque accumulation at the base of the implant, which triggers an immune response. This response, according to experts, leads to inflammation, bleeding, and bone loss. If left untreated, peri-implantitis can result in implant failure and loss of the supporting bone.
What are the Signs and Symptoms of Peri-Implantitis?
Peri-implantitis can be difficult to detect in its early stages, as it may not cause any pain or discomfort. However, some of the signs and symptoms that you should look out for include:
- Redness, swelling, or tenderness of the gums around the implant
- Bleeding or pus when brushing or probing the implant site
- Loosening or shifting of the implant or the crown, bridge or denture
- Exposed metal threads or implant components
- Bad breath or unpleasant taste in the mouth
- Difficulty chewing or biting
If you notice any of these signs or symptoms, you should contact your dental implant specialist as soon as possible for an evaluation and treatment.
What Can Cause Peri-Implantits?
Although research has shown that the success rate of dental implants is 97% ten years after the procedure, the most common complication for the implants that fail is PI. It’s important to note that it has been found that approximately 22% of dental implant patients with periodontitis (gum disease) develop peri-implantitis.
In general, however, PI is a complex condition that can have multiple causes and contributing factors that can increase the risk of developing peri-implantitis, such as:
- Lifestyle choices such as alcohol consumption and smoking impair healing and increase infection risk by affecting the blood supply and the immune system.
- Systemic diseases, like diabetes which affects the immune system, making it harder to control inflammation and infection, or drug therapies that can affect bone density.
- Obesity increases the risk because it leads to ongoing inflammation throughout the body. This inflammation can disrupt the immune system by causing more of the chemicals that promote inflammation to be produced. This, in turn, can harm the health of your gums and the bones that hold your teeth.
- As we have already mentioned, patients who have had periodontitis in the past are more likely to have residual bacteria and inflammation in their oral tissues, which can affect the implant site.
- Not brushing and flossing teeth and implants daily and not using antibacterial mouthwash as recommended make it more likely to have plaque buildup and inflammation around dental implants.
- Patients who have thin or insufficient gum tissue around their implants are more prone to infection and bone loss, as they have less protection and support for the implant.
- Having poor bone quality or density makes it more likely to have implant instability and bone loss, due to less anchorage and resistance for the implant.
- Implants that have rough surfaces or are placed too deep may harbor more bacteria and cause more inflammation and bone loss than implants that have smooth surfaces or are placed at the optimal depth.
- Improper restorative design, occlusal overload, micro gaps, and residual cement can also cause peri-implantitis by creating mechanical stress, bacterial leakage, or foreign body reactions around the implant.
These factors can interact with each other and influence the development and progression of PI. Therefore, it is important to identify and control these factors before and after getting your dental implants.
How to Help Prevent Peri-Implantitis?
The best way to prevent PI is to maintain good oral hygiene and follow your dental implant specialist’s aftercare instructions. Some of the preventive measures that you can take include:
- Brushing your teeth twice a day with a soft-bristled toothbrush and a fluoride toothpaste
- Flossing daily or using other interdental cleaning aids such as water flossers or interdental brushes
- Rinsing your mouth with an antibacterial mouthwash as recommended by your dentist
- Visiting your dentist regularly for check-ups and professional cleanings
- Avoiding smoking, alcohol consumption, and other habits that can impair healing and increase infection risk
- Controlling any systemic conditions that can affect your oral health such as diabetes or osteoporosis
How to Treat Peri-Implantitis?
If you have been diagnosed with peri-implantitis, you should seek treatment as soon as possible to avoid further damage and complications. The treatment of PI depends on the severity and extent of the infection and bone loss. Some of the treatment options that your dental implant specialist may suggest include:
Non-Surgical Treatment
This involves removing the plaque and calculus from the implant surface and the surrounding tissues using mechanical or chemical methods. Your dentist may also prescribe antibiotics, antiseptics, or anti-inflammatory drugs to control the infection and inflammation.
Surgical Treatment
This involves opening up the gum tissue around the implant and cleaning the infected area. Your dentist may also perform bone grafting or guided tissue regeneration to restore the lost bone and support the implant. In some cases, your dentist may need to remove and replace the implant if it is too damaged or loose.
Laser Therapy
This involves using a low-intensity laser beam to kill the bacteria and stimulate the healing of the tissues around the implant. Laser therapy can be used alone or in combination with other treatments.
Why Choose Dr Ghodsi for Your Dental Implants in Las Vegas and Pasadena?

If you are looking for a dental implant specialist who can provide you with high-quality care and results, contact Dr Ghodsi at Lasting Smiles Dental Care in Las Vegas and Pasadena. Dr Ghodsi has over 30 years of experience and has performed more than 10,000 successful dental implant procedures. He has his own in-house lab, state-of-the-art facility dental clinic, 3D imaging technology and uses guided implant placement which significantly increase the likelihood that every dental implant procedure is performed with precision and efficiency, in order to minimize the possibility of complications such as PI.
Dr Ghodsi offers affordable pricing, payment and financing options, and free virtual consultations. He and his team are committed to providing you with personalized attention, compassionate care, and exceptional results. They will guide you through every step of your dental implant journey, from consultation to aftercare, and ensure that you are comfortable and satisfied with your new smile.
Don’t let missing teeth or peri-implantitis ruin your smile and your confidence. Contact us today at (702) 259-5295 for Las Vegas or (626) 325-6000 for Pasadena to schedule your appointment with Dr Ghodsi and find out how dental implants can transform your life.




